Between the vertebrae of the spine, there are openings through which the spinal nerve roots pass to exit the spinal column, called foramen. Foraminal stenosis is a condition in which one or more of the vertebral foramen narrows, impinging on or “pinching” the spinal nerve roots.
What Is Foraminal Stenosis?
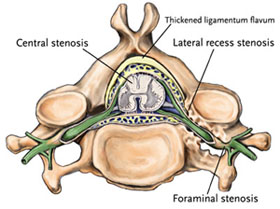
Foraminal stenosis is a condition in which one or more of the vertebral foramen narrows, impinging on or “pinching” the spinal nerve roots. It may be caused by a variety of conditions, most of which are associated with degenerative changes in the spine. These include:
- A herniated or bulging disc
- Arthritis
- Bone spurs
- Ligament thickening
- Scar tissue
- Spinal joint enlargement
Because spinal stenosis is so often precipitated by spinal degeneration, it’s most commonly found in patients age 50 or over; however, genetics and congenital conditions also may be a factor.
What Are The Symptoms of Foraminal Stenosis?
The symptoms of foraminal stenosis may include one or more of the following:
- Back or neck pain that tends to worsen progressively rather than develop suddenly.
- Radiating pain that extends into other parts of the body
- Numbness
- Weakness
- Burning, tingling (“pins and needles”) sensation
How Is Foraminal Stenosis Diagnosed?
To determine whether you have foraminal stenosis, your provider will examine your back and your medical history, and may order an x-ray, computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of your spine.
How Is Foraminal Stenosis Treated?
If there is minimal nerve involvement and your symptoms are mild and do not interfere with daily life, your provider may prescribe one or more of the following conservative therapies to treat your condition.
- Medication — Over-the-counter medications such as a non-steroidal anti-inflammatory drug (NSAID) or, if this fails to provide relief, a prescription pain reliever, steroid or muscle relaxer.
- Posture correction — Proper alignment of the spine can reduce stress on the lower back and neck.
- Activity modification — Altering the home and workplace to eliminate excessive twisting, stretching, and bending, as well as learning proper lifting techniques.
- Exercise/physical therapy — To improve flexibility, strength and circulation, as well as reduce pain and inflammation and increase pain-free movement.
- External bracing — To support the spine during the healing process.
If conservative treatment fails to provide lasting relief, your provider may recommend spine surgery to remove the source of pressure on the spinal nerve roots. Surgical therapies for treating foraminal stenosis include:
- Laminectomy — A procedure in which the lamina of the affected vertebrae (the portion of the vertebral arch that forms the “roof” of the spinal canal) is removed or trimmed to widen the foramen and create more space for the spinal nerves.
- Anterior cervical discectomy with fusion — A procedure in which the intervertebral disc is removed and the disc space distracted to “re-open” the foramen and give the nerve roots more room, and the vertebrae then joined together (fused) by placing bone graft between the affected levels. The graft material acts as a binding medium and also helps to maintain normal disc height – as the body heals, the vertebral bone and bone graft eventually grow together to join the vertebrae and stabilize the spine.
These procedures may be performed using traditional, “open” or minimally invasive surgical techniques, depending on your condition and your provider’s preference, experience and training.
The decision to treat foraminal stenosis surgically requires careful consideration between you and your provider. Factors to be considered are your specific condition and overall physical health. Discuss your condition thoroughly with your provider, and rely on his or her judgment regarding which treatment option is most appropriate.

